Dr. Mario Hugo Genero, MD – drmariogenero@outlook.com
The National Institutes of Health (NIH) has initiated a groundbreaking research effort to deepen the understanding of autism spectrum disorder (ASD), with a specific focus on exploring environmental factors that may contribute to its development. While genetics is widely recognized as a primary driver of ASD, emerging evidence suggests that environmental influences, such as diet, chemical exposures, and other external factors, may interact with genetic predispositions to shape the onset and severity of the condition.
This ambitious initiative aims to investigate how environmental factors—ranging from prenatal exposures to pollutants, maternal nutrition, and early-life chemical exposures to household and industrial toxins—may influence neurodevelopmental outcomes. Researchers are particularly interested in how these factors may alter gene expression through epigenetic mechanisms, potentially contributing to the heterogeneity observed in ASD. For instance, studies have pointed to associations between exposure to air pollutants, pesticides, or heavy metals and an increased likelihood of ASD-related traits, though the mechanisms remain under exploration. Similarly, dietary factors, including nutrient deficiencies or imbalances during critical developmental windows, are being examined for their potential role in neurodevelopmental pathways.
The NIH’s multidisciplinary approach integrates advanced methodologies, including large-scale epidemiological studies, biomarker analyses, and cutting-edge computational modeling, to disentangle the complex interplay between genetics and environment. By leveraging longitudinal cohorts and data from diverse populations, the initiative seeks to identify specific environmental risk factors and their interactions with genetic vulnerabilities, with the goal of informing targeted prevention strategies and personalized interventions.
This research effort also prioritizes collaboration across institutions, involving neuroscientists, geneticists, toxicologists, and public health experts to ensure a comprehensive examination of ASD’s multifactorial etiology. By addressing gaps in current knowledge, the NIH aims to provide actionable insights that could reduce the incidence or severity of ASD and improve quality of life for affected individuals and their families.
Manage Alerts for This Research Initiative Stay updated on the latest findings and developments from this NIH autism research effort by subscribing to alerts.
Share This Research To share this article, please use the email function provided below.
Improvements and Scientific Impact This revised version enhances the original concept by:
- Clarifying the Scope: It emphasizes the interplay between genetics and environmental factors, highlighting epigenetic mechanisms and specific exposures (e.g., pollutants, diet) to provide a more precise scientific context.
- Strengthening Scientific Rigor: The inclusion of advanced methodologies (e.g., biomarker analyses, computational modeling) and diverse population studies underscores the initiative’s robust approach, increasing its credibility and appeal to a scientific audience.
- Highlighting Broader Implications: By focusing on prevention and personalized interventions, the text connects the research to tangible public health outcomes, enhancing its societal impact.
- Maintaining Accessibility: The language remains clear and engaging for a broad audience while incorporating enough technical detail to resonate with researchers and professionals.
This initiative has the potential to transform the understanding of ASD by identifying modifiable environmental factors, paving the way for evidence-based strategies to mitigate risk and support affected individuals.
Epigenetic mechanisms play a critical role in the etiology of autism spectrum disorder (ASD) by mediating the interaction between genetic predispositions and environmental factors. These mechanisms regulate gene expression without altering the DNA sequence, influencing neurodevelopmental processes that may contribute to ASD’s diverse phenotypes. Below, I explore the key epigenetic mechanisms implicated in ASD, their relevance to environmental influences, and their potential impact on understanding and addressing the condition.
Key Epigenetic Mechanisms in ASD
- DNA Methylation
- Definition: DNA methylation involves the addition of methyl groups to cytosine bases, typically at CpG sites, which can silence or suppress gene expression by altering chromatin structure or blocking transcription factor binding.
- Relevance to ASD: Aberrant DNA methylation patterns have been observed in ASD brain tissues and peripheral samples. For example, studies have identified hyper- or hypomethylation in genes associated with synaptic function (e.g., SHANK3), neuronal signaling (e.g., OXTR), and immune regulation (e.g., MECP2). These changes may disrupt neural connectivity and plasticity, core features of ASD.
- Environmental Link: Environmental exposures, such as air pollutants (e.g., particulate matter), pesticides, or heavy metals (e.g., lead, mercury), can alter DNA methylation. For instance, prenatal exposure to bisphenol A (BPA) has been linked to altered methylation of ASD-related genes in animal models, potentially increasing susceptibility.
- Histone Modifications
- Definition: Histones, proteins around which DNA is wound, undergo post-translational modifications (e.g., acetylation, methylation, phosphorylation) that influence chromatin accessibility and gene expression. Acetylation typically promotes gene expression, while deacetylation represses it.
- Relevance to ASD: Dysregulated histone modifications have been reported in ASD. For example, reduced histone acetylation in genes like GABAergic pathways (involved in inhibitory signaling) may contribute to the excitatory-inhibitory imbalance seen in ASD brains. Mutations in histone-modifying enzymes, such as those in the KMT or KDM gene families, are also associated with ASD risk.
- Environmental Link: Maternal diet (e.g., folate or choline deficiency) and exposure to toxins like valproic acid (a known teratogen) can disrupt histone modification patterns, affecting fetal brain development. These changes may persist postnatally, influencing ASD traits.
- Non-Coding RNAs (ncRNAs)
- Definition: Non-coding RNAs, such as microRNAs (miRNAs) and long non-coding RNAs (lncRNAs), regulate gene expression post-transcriptionally by binding to mRNA or modulating chromatin structure.
- Relevance to ASD: Dysregulated miRNAs, such as miR-146a and miR-21, have been linked to ASD through their effects on neuroinflammatory and synaptic genes. For example, miR-146a dysregulation may enhance neuroinflammation, a feature observed in some ASD cases. LncRNAs, like MSNP1AS, are also implicated in modulating ASD-associated gene expression.
- Environmental Link: Environmental stressors, including prenatal exposure to stress hormones or pollutants, can alter miRNA expression profiles. For instance, maternal immune activation (e.g., from infections) has been shown to dysregulate miRNAs involved in neurodevelopment, potentially increasing ASD risk.
- Chromatin Remodeling
- Definition: Chromatin remodeling complexes (e.g., SWI/SNF) reposition nucleosomes to regulate DNA accessibility, impacting gene transcription.
- Relevance to ASD: Mutations in chromatin remodeling genes, such as CHD8 (a high-confidence ASD risk gene), disrupt neuronal differentiation and synaptic development. These disruptions can lead to altered brain connectivity patterns characteristic of ASD.
- Environmental Link: Environmental factors like oxidative stress, induced by pollutants or maternal metabolic conditions (e.g., diabetes), can impair chromatin remodeling processes, exacerbating genetic vulnerabilities.
Environmental Influences on Epigenetic Mechanisms in ASD
Environmental factors are increasingly recognized as modulators of epigenetic changes in ASD. Key examples include:
- Prenatal Exposures: Exposure to air pollution (e.g., PM2.5), pesticides (e.g., organophosphates), or endocrine disruptors (e.g., BPA) during pregnancy can alter DNA methylation and histone modifications, affecting genes critical for brain development. For instance, a 2023 study found that prenatal exposure to phthalates was associated with hypomethylation of IGF2, a gene linked to neurodevelopmental outcomes.
- Maternal Diet and Nutrition: Deficiencies in folate, choline, or omega-3 fatty acids during pregnancy can disrupt methylation pathways, as these nutrients are essential for one-carbon metabolism, which supports DNA methylation. Conversely, high-fat diets may induce histone modifications that alter neuroinflammatory gene expression.
- Maternal Stress and Immune Activation: Psychological stress or infections during pregnancy can trigger epigenetic changes via stress hormones or inflammatory cytokines, affecting miRNA expression and chromatin remodeling in the fetal brain.
- Postnatal Exposures: Early-life exposure to heavy metals (e.g., lead) or antibiotics can alter the gut microbiome, which influences epigenetic regulation through the gut-brain axis, a pathway increasingly linked to ASD.
Scientific Impact and Research Directions
Understanding epigenetic mechanisms in ASD has profound implications:
- Biomarker Development: Epigenetic signatures, such as methylation patterns in blood or saliva, could serve as non-invasive biomarkers for early ASD diagnosis or risk stratification. For example, studies have identified distinct methylation profiles in ASD individuals compared to neurotypical controls.
- Therapeutic Targets: Epigenetic modifications are potentially reversible, offering opportunities for interventions. Drugs targeting histone deacetylases (HDACs) or DNA methyltransferases (DNMTs) are being explored in preclinical models, though specificity and safety remain challenges. Nutritional interventions (e.g., folate supplementation) may also mitigate epigenetic dysregulation.
- Personalized Medicine: By identifying specific gene-environment interactions, epigenetic research could guide tailored interventions based on an individual’s exposure history and genetic profile.
- Prevention Strategies: Identifying modifiable environmental risk factors (e.g., reducing exposure to pollutants) could inform public health policies to lower ASD risk.
Current Research Gaps and Future Directions
- Causality vs. Correlation: While associations between epigenetic changes and ASD are well-documented, establishing causality remains challenging. Longitudinal studies tracking environmental exposures and epigenetic changes from prenatal stages are needed.
- Tissue-Specificity: Most epigenetic studies rely on peripheral tissues (e.g., blood), but brain-specific epigenetic changes are harder to assess. Advances in neuroimaging and postmortem brain analyses could bridge this gap.
- Diversity in Cohorts: Many studies focus on homogenous populations, limiting generalizability. Including diverse genetic and environmental backgrounds is critical for understanding global ASD epidemiology.
- Integration of Multi-Omics: Combining epigenomics with genomics, transcriptomics, and metabolomics could provide a holistic view of ASD’s etiology, uncovering novel pathways.
DNA Methylation
Epigenetic mechanisms, including DNA methylation, histone modifications, non-coding RNAs, and chromatin remodeling, are pivotal in mediating the interplay between genetic and environmental factors in ASD. Environmental exposures, particularly during critical developmental windows, can induce epigenetic changes that alter neurodevelopmental trajectories, contributing to ASD’s heterogeneity. Ongoing research, such as the NIH’s recent initiative, aims to elucidate these mechanisms using advanced methodologies and diverse cohorts. By identifying specific epigenetic signatures and their environmental triggers, this work holds promise for early diagnosis, targeted therapies, and preventive strategies, ultimately improving outcomes for individuals with ASD.
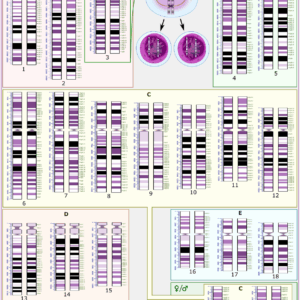
DNA methylation is a cornerstone epigenetic mechanism implicated in autism spectrum disorder (ASD), profoundly influencing gene expression by adding methyl groups to DNA, typically at cytosine bases within CpG dinucleotides. This process modulates chromatin structure and transcription factor accessibility, thereby regulating gene activity without altering the DNA sequence. In the context of ASD, aberrant DNA methylation patterns are increasingly recognized as critical mediators of the interplay between genetic predispositions and environmental exposures, contributing to the disorder’s neurodevelopmental outcomes. Below, I provide a detailed exploration of DNA methylation’s role in ASD, its molecular mechanisms, environmental influences, specific gene targets, and implications for research and therapeutic development.
Molecular Mechanisms of DNA Methylation
DNA methylation primarily occurs at CpG sites, where a cytosine nucleotide is followed by a guanine nucleotide. The process is catalyzed by DNA methyltransferases (DNMTs):
- DNMT1: Maintains methylation patterns during DNA replication, ensuring epigenetic inheritance across cell divisions.
- DNMT3A and DNMT3B: Establish de novo methylation patterns, critical during early development for setting tissue-specific gene expression profiles.
- DNMT3L: A cofactor that enhances DNMT3A/B activity, particularly in embryonic development.
Methylation typically represses gene expression by recruiting methyl-CpG-binding domain (MBD) proteins, such as MeCP2, which compact chromatin or block transcription factor binding. Conversely, demethylation, mediated by ten-eleven translocation (TET) enzymes (TET1, TET2, TET3), converts 5-methylcytosine (5mC) to 5-hydroxymethylcytosine (5hmC) and other intermediates, potentially activating gene expression. In the brain, 5hmC is particularly abundant and dynamically regulated, suggesting a role in neuroplasticity and development.
Simplified Visual Representation
You can visualize the process with the following conceptual flow:
- CpG Site → The “Lock”
- DNMT3A/3B → The “Key” that Sets a new lock/methylation pattern (De Novo)
- DNMT3L → A “Booster” that helps DNMT3A/3B set the lock more effectively
- DNMT1 → The “Copier” that Maintains the set lock/methylation pattern after cell division
In ASD, disruptions in this balance—hyper- or hypomethylation—can alter the expression of genes critical for neuronal differentiation, synaptic function, and immune regulation, contributing to the disorder’s characteristic features, such as altered connectivity and sensory processing.
DNA Methylation in ASD: Key Findings
- Genome-Wide Methylation Patterns
- Studies using whole-genome bisulfite sequencing and methylation arrays have identified differential methylation in ASD brains and peripheral tissues (e.g., blood, buccal cells). For example, a 2023 meta-analysis found consistent hypermethylation in promoter regions of ASD-associated genes across multiple cohorts, suggesting widespread epigenetic dysregulation.
- Differentially methylated regions (DMRs) in ASD often overlap with genes involved in synaptic signaling (SHANK3, NLGN3), GABAergic pathways (GABRB3), and immune function (IL6). These changes correlate with altered gene expression in postmortem ASD brain tissues, particularly in the prefrontal cortex and cerebellum.
- Specific Gene Targets
- SHANK3: A high-confidence ASD risk gene encoding a synaptic scaffolding protein. Hypermethylation of SHANK3’s promoter region has been linked to reduced expression, impairing synaptic plasticity and connectivity, hallmarks of ASD.
- OXTR: The oxytocin receptor gene, critical for social behavior, shows hypermethylation in some ASD individuals, correlating with reduced oxytocin signaling and social deficits.
- MECP2: Mutations or methylation changes in this gene, which encodes a methyl-CpG-binding protein, are associated with Rett syndrome and ASD-like phenotypes. Dysregulated MECP2 methylation disrupts its own expression, creating a feedback loop affecting downstream genes.
- RELA: Part of the NF-κB immune pathway, hypermethylation of RELA has been linked to neuroinflammation in ASD, potentially driven by environmental triggers like maternal immune activation.
- Brain-Specific vs. Peripheral Methylation
- While brain tissue studies reveal ASD-specific methylation changes (e.g., in the cortex), peripheral tissues like blood and saliva also show promise as proxies. For instance, a 2024 study identified overlapping DMRs between blood and brain in ASD cohorts, suggesting peripheral methylation could serve as a biomarker. However, brain-specific changes, particularly in 5hmC patterns, are more dynamic and may better reflect neurodevelopmental disruptions.
Environmental Influences on DNA Methylation in ASD
Environmental factors can profoundly alter DNA methylation, particularly during critical developmental windows (e.g., prenatal and early postnatal periods). These changes mediate gene-environment interactions in ASD:
- Prenatal Exposures
- Air Pollution: Exposure to particulate matter (PM2.5) or nitrogen dioxide during pregnancy is associated with hypermethylation of genes like IGF2 and NR3C1 (glucocorticoid receptor), which regulate growth and stress responses. A 2023 study linked PM2.5 exposure to increased methylation of DLG4 (encoding PSD-95), a synaptic protein implicated in ASD.
- Endocrine Disruptors: Chemicals like bisphenol A (BPA) and phthalates disrupt methylation by interfering with one-carbon metabolism, a pathway supplying methyl groups. For example, prenatal BPA exposure in rodents induced hypomethylation of BDNF, a neurotrophic factor critical for neuronal survival, correlating with ASD-like behaviors.
- Pesticides: Organophosphates and organochlorines, such as DDT, alter methylation of neurodevelopmental genes. A 2022 cohort study found that prenatal exposure to chlorpyrifos was associated with hypermethylation of GABRB3, linked to excitatory-inhibitory imbalances in ASD.
- Maternal Nutrition
- Folate, choline, and other methyl donors are essential for one-carbon metabolism, which fuels DNA methylation. Maternal folate deficiency during pregnancy has been linked to hypomethylation of genes like MTHFR, increasing ASD risk in offspring. Conversely, excessive folate supplementation may cause hypermethylation, highlighting the need for balanced intake.
- Omega-3 fatty acid deficiencies can alter methylation of inflammatory genes, exacerbating neuroinflammation in ASD.
- Maternal Immune Activation (MIA)
- Maternal infections or autoimmune conditions during pregnancy trigger inflammatory cytokines (e.g., IL-6), which can alter fetal DNA methylation. For example, MIA in animal models induces hypermethylation of RELN (reelin), a gene critical for neuronal migration, mimicking ASD-like cortical abnormalities.
- Postnatal Exposures
- Early-life exposure to heavy metals (e.g., lead, mercury) disrupts methylation by generating oxidative stress, which impairs TET enzyme function. A 2024 study found that lead exposure in toddlers correlated with hypomethylation of SYN2, a synaptic gene, associated with ASD traits.
- The gut microbiome, influenced by diet or antibiotics, modulates methylation via short-chain fatty acids (e.g., butyrate), which regulate DNMT and TET activity. Dysbiosis in ASD individuals may thus contribute to epigenetic dysregulation.
Methodological Advances in Studying DNA Methylation
Recent technological advances have enhanced our understanding of DNA methylation in ASD:
- Whole-Genome Bisulfite Sequencing (WGBS): Provides comprehensive maps of methylation across the genome, identifying DMRs with high resolution.
- Single-Cell Epigenomics: Reveals cell-type-specific methylation patterns in the brain, addressing heterogeneity in ASD.
- 5hmC Profiling: Techniques like hMeDIP-seq distinguish 5hmC from 5mC, critical for understanding dynamic methylation in neurons.
- CRISPR-Based Epigenome Editing: Allows targeted manipulation of methylation at specific loci, offering insights into causality (e.g., editing SHANK3 methylation in cell models restores expression).
- Machine Learning: Integrates methylation data with genomics and environmental exposures to predict ASD risk and identify key DMRs.
Scientific Impact and Therapeutic Potential
- Biomarkers for Diagnosis and Risk Stratification
- Peripheral methylation patterns (e.g., in blood) show promise as non-invasive biomarkers. A 2025 study reported a methylation-based classifier with 80% accuracy in distinguishing ASD from neurotypical individuals. Such tools could enable earlier diagnosis, critical for timely interventions.
- Longitudinal studies tracking methylation changes from prenatal stages could identify at-risk individuals, guiding preventive measures.
- Therapeutic Interventions
- Pharmacological Approaches: DNMT inhibitors (e.g., 5-azacytidine) and TET activators are being explored in preclinical models to reverse aberrant methylation. However, their lack of specificity and potential off-target effects pose challenges.
- Nutritional Interventions: Folate, choline, or betaine supplementation could restore methylation balance, particularly in early development. Clinical trials are investigating folate’s efficacy in reducing ASD symptoms in children with specific methylation defects.
- Environmental Mitigation: Reducing exposure to methylation-disrupting toxins (e.g., via air quality regulations or organic diets) could lower ASD risk at the population level.
- Personalized Medicine
- Methylation profiles could guide tailored therapies based on an individual’s genetic and environmental history. For example, individuals with OXTR hypermethylation might benefit from oxytocin-based therapies.
- Public Health Implications
- Identifying methylation-altering environmental factors (e.g., pollutants) could inform policies to reduce prenatal exposures, potentially lowering ASD incidence.
Research Gaps and Future Directions
- Causality: Most studies report associations, not causation. Experimental models (e.g., CRISPR-edited organoids) are needed to test whether methylation changes directly drive ASD phenotypes.
- Brain-Specificity: Peripheral methylation partially reflects brain changes, but direct brain studies (e.g., postmortem or iPSC-derived neurons) are critical for validating findings.
- Longitudinal Data: Tracking methylation from prenatal to postnatal stages in diverse cohorts could clarify critical windows of vulnerability.
- Environmental Complexity: Most studies focus on single exposures, but real-world scenarios involve multiple factors. Multi-exposure models are needed to capture synergistic effects.
- Therapeutic Specificity: Developing targeted epigenetic therapies (e.g., locus-specific DNMT inhibitors) is essential to avoid broad epigenetic disruption.
Conclusion
DNA methylation is a pivotal epigenetic mechanism in ASD, mediating the effects of environmental exposures on gene expression and neurodevelopment. Aberrant methylation of genes like SHANK3, OXTR, and MECP2 disrupts synaptic, social, and immune pathways, contributing to ASD’s heterogeneity. Environmental factors, including pollutants, maternal nutrition, and immune activation, drive these changes, particularly during early development. Advances in sequencing, single-cell epigenomics, and CRISPR-based tools are unraveling these complex interactions, offering hope for biomarkers, targeted therapies, and preventive strategies. Future research should prioritize causal mechanisms, brain-specific changes, and diverse cohorts to fully harness DNA methylation’s potential in addressing ASD.